Interview: Urine self sampling could change the world of testing, not only for HPV but also for other oncology markers
Our own Rebecca Millecamps, Marketing Manager at Fujirebio, was interviewed for the podcast series 'Molecules, microbes and multiomics' about the importance of HPV testing and urine self sampling. Listen to the interview in the video below or read the full transcription further down on this page.
Why is testing for HPV important?
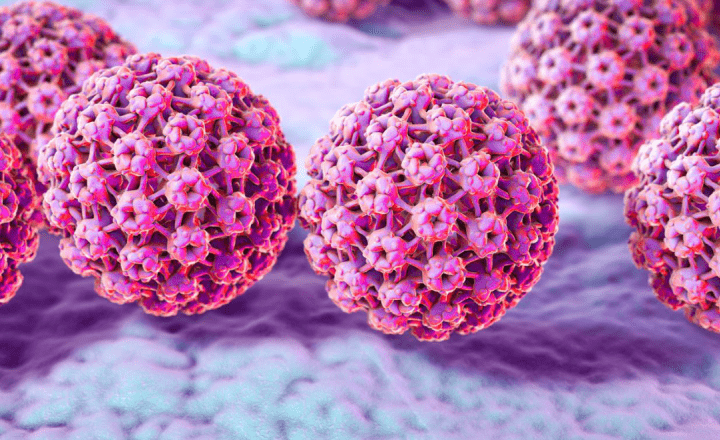
Rebecca Millecamps: When you talk about HPV, you talk about cervical cancer. Worldwide cervical cancer is the fourth most common cancer in woman with an estimation of 300 000 deaths worldwide.1
I think these numbers are shocking, knowing that cervical cancer can be prevented. On the one hand you have primary prevention aiming on education and vaccination. The secondary prevention means early diagnosis and early treatment.
It is known that virtually all cervical cancers are caused by the human papillomavirus. There are two determinative factors when it comes to cervical cancer: One: the HPV genotype and two: the persistence of the HPV infection. Type+time=risk.
Knowing the genotype and the persistence of infection, so knowing how long the infection with that particular genotype is already ongoing, gives a very good estimate of the risk to develop a cervical cancer.
The good news is that cervical cancer can be prevented, and is also highly curable when it is diagnosed and treated early.
The bad news is that most cases of cervical cancer occur in women who are not regularly screened and not treated on a timely basis.1
So, ensuring women are adequately screened and treated is critical to reduce deaths from cervical cancer.2
Today, screening today is based on cytology and HPV testing with a clear trend towards HPV-based primary screening.
What are the challenges surrounding HPV screening?
The challenge is the participation rate.
If 100% of the women would participate in screening, the impact on the prevention of cervical cancer would be significant.
Unfortunately, that is not the case today.
Looking at Europe, in some countries up to 40% of the women does not participate in the screening programs.
On a worldwide level, screening coverage is dramatically low in some countries where only 20, 30 – 40% of the women participate.2
There are different reasons why women do not participate.
Today, cervical cytology (the so-called PAP test) is still considered the gold standard for cervical cancer screening. The cervical sample which is used for cytology, is also used for HPV testing.
But the invasive nature of cervical sampling is often disliked by women. They feel discomfort or embarrassment with the pelvic examinations. It is also perceived as time consuming because woman need to take time of work, to attend an appointment with a clinician. Religion or culture can also play an important role.
In some countries or regions, they do not have the necessary facilities or have limited transportation options to get a cervical sample collected and afterwards tested.3
Or another reason is that simply women don’t think they need screening for one reason or the other.
Can these challenges be overcome?
Yes. We believe they can.
When looking at reasons for a poor screening uptake, one of the solutions could be to offer non-invasive self-sampling methods to collect the sample.
Both cervicovaginal and urine self-sampling devices or methods have been proven effective in increasing participation and screening coverage of target populations.4
What is the added value of Fujirebio’s INNO-LiPA® HPV Genotyping Extra II?
The added value of the INNO-LiPA HPV Genotyping assay is the high sensitivity and specificity
Our assay has been widely demonstrated to generate sensitive and specific results, identifying up to 32 genotypes simultaneously in cervical swab samples and in paraffin-embedded tissue.
By using the SPF10 PCR target, the INNO-LiPA HPV assay can identify HPV infections even at a low viral load, also in mixed HPV infections.5,6,7
Why did Fujirebio decide to validate urine sampling for HPV testing?
There is clearly a trend towards self-sampling. So we anticipate, by offering the possibility to perform full HPV genotyping also on first void urine samples.
Urine sampling overcomes the different barriers for woman when it comes clinician taken samples. It offers a more comfortable sampling which is less time consuming and could be more acceptable looking at social, cultural or religious reasons.
Several studies show that HPV DNA can be detected in urine samples using sensitive HPV DNA assays.8,9,10
The high analytical sensitivity of the INNO-LiPA assay allows an almost equivalent performance on both cervical and first-void urine samples, despite the lower viral load present in urine compared to cervical samples. At Fujirebio we optimized and standardized the pre-analytical protocol eliminating the need for a concentration step of the sample before DNA extraction. We consider this as a plus for the testing lab as it reduces the overall turn around time. (Reference: IFU of INNO-LiPA HPV Genotyping Extra II)
Why is it important to genotype HPV infections?
Identifying the HPV genotype offers the ability to look at the persistence of an infection with the same HPV genotype. Knowing the genotype ánd the persistence of infection, gives the best estimate of the risk to develop a cervical cancer. Type+time=risk.
With limited High Risk HPV screening only you can not see if the same HPV genotype is found in consecutive samples.
Genotype information can lead to optimization of risk-based triage strategies.
The efficacy and impact of screening programs and vaccination programs needs to be checked. Evaluating the HPV prevalence and genotype distribution is important to keep track of the association of different HPV genotypes with cervical cancer.
There is still a need to improve the understanding of the carcinogenic nature of individual HPV genotypes. Continued research is needed to fill the gaps in understanding the individual-level HPV natural history to guide patient counselling about the HPV test results.
Data needs to be collected on the geographic prevalence of the different HPV genotypes, in association with the full spectrum from normal cytology to invasive cervical cancer to understand the relative carcinogenic potential of the different HPV genotypes.11
What is the benefit of performing HPV genotyping in urine samples?
Thanks to the high sensitivity and the possibility to identify up to 32 genotypes, the INNO-LiPA HPV Genotyping assays is used a lot in epidemiological studies, post-vaccination monitoring and clinical trials for new HPV vaccines.
Self-collected samples are likely to become part of HPV screening but also for post-vaccination monitoring and epidemiological programs this is a promising approach.8,12
An easier way to collect samples will make these programs easier to organise, less-costly, more efficient and we believe as such more impactful.
Self-collection of urine proved to be highly acceptable in vaccine impact studies conducted by the World Health Organization (WHO) and International Agency for Research on Cancer (IARC). It allowed a high-throughput of sample collection with minimal requirements for trained staff.14
HPV is not only related to cervical cancer but also to many other cancers such as vaginal cancer and urethral cancer. So also in this context, knowing the involved HPV genotypes is important to evaluate for example the impact of HPV vaccination also on the prevalence of these other cancers.13
How will urine testing impact HPV testing?
Most cases of cervical cancer occur in women who are not screened on a regular basis. So, making sure women are adequately screened and treated is critical to reduce deaths from cervical cancer. Offering easy to handle self-sampling methods will definitely make HPV testing more accessible to patients and healthcare professionals. A significant number of women today have almost no access to early diagnosis and treatment, for example people with a low socioeconomic status or living in remote areas with poor access to healthcare services.
A urine sample can be collected easily without the need for a clinician and sent by regular mail to the lab for testing.
But protecting the sample from degradation is important. Either immediately freezing the sample or mixing with a preservative is important. A standardized and easy to handle method to collect the sample is important to guarantee that the sample has a good quality and is useful for testing.
Several investigations and surveys have been done already looking at self sampling. Clearly women prefer a non-invasive sampling method.
Talking to healthcare professionals, there is a strong believe that this could have a huge impact on screening uptake.15,16
Looking at self-sampling in general, women may have concerns about self-sampling using vaginal brushes. They are worried to hurt themselves or they are concerned about not getting a good sample. In some populations there is an unwillingness to touch the genital region. Or woman are inable to see their own genital area while taking the self-sample.17
Looking at these concerns, taking a urine sample using the Colli-Pee is less complicated and easier to do and might be more accepted by women compared to other self-sampling methods.
What are the challenges with urine collection?
As is the case for all samples, also for urine it is important to ensure good quality and a sufficient amount of DNA for testing.
HPV in urine comes from debris, exfoliated cells coming from the cervix, and from vaginal epithelial cells. When urinating, the urine flow washes away this material. Obviously, the first stream or void contains most cells and HPV DNA.
In practice, it is not easy to collect only the first part of the urine flow. It is difficult to stop the urine flow on time.
So the challenge with urine collection is to have a standardized urine collection of only the first part of the urine flow, in an easy and hygienic way.
Next to that, optimal storage of the urine sample is important to ensure good quality of the sample up to the time of testing.
To ensure good quality, either the urine sample should be frozen immediately, or it should be mixed immediately with a preservative to prevent HPV DNA degradation.18,19,20
Can a randomly collected urine sample be used?
Preferably, the urine sample for HPV testing consists of first-void urine because this first void or urine contains a larger amount of HPV DNA when you compare to random or midstream sampling.
Using first-void urine enables a more sensitive and a more accurate detection of cervical HPV.18,19,20
How important is it to use first-void (first-catch) urine?
It is important to use the first catch to ensure most reliable, optimal results.
Using other urine sample, most probably still HPV will be detectable, especially using a highly sensitive assay such as the INNO-LiPA.
However, in case of very low viral loads and in mixed HPV infections, it is possible that the HPV will not be detected when using a more diluted sample because a higher volume of urine was collected and not only the first void.18,19,20
Why did you choose to partner with Novosanis and their Colli-Pee device?
A good result needs a good sample.
Our passion at Fujirebio is to bring good quality health care solutions to the labs, doctors, and patients.
Obtaining a reliable result does however also depend on the quality of the sample taken.
Several variables can affect the HPV genotyping results: sample collection and preservation, DNA extraction, and the method used for HPV DNA detection and genotyping.
We want to standardize these variables and offer a robust method for HPV detection and genotyping. Therefore, we decided to work with first void urine and offer the Colli-Pee as a urine collection device in combination with our INNO-LiPA HPV assay.18,20
What does it mean for labs and patients to have a CE-IVD solution for HPV genotyping in urine?
There is clearly a trend towards self-sampling. Fujirebio anticipates. By offering already the possibility to perform reliable full HPV genotyping on first void urine samples.
Having a CE-IVD method means that the INNO-LiPA has been validated for giving reliable HPV genotyping results also starting from urine samples. Now the protocol is CE certified, labs do not have to perform themselves extensive validation themselves to offer urine analysis for HPV.
How do you see the future for urine testing for HPV compared to cervical sample?
There is strong belief that urine sampling could change the world of testing, not only for HPV but also for other oncology markers. Fujirebio is looking into evaluation of HE4, a marker for ovarian cancer, in urine sample.
In general, there is clearly a trend towards self-sampling.
But there are still some challenges to overcome and some gaps to fill. There is a need for education and awareness programs to make patients and clinicians more familiar with HPV testing in urine. Studies are continuously ongoing to generate more data and to create more awareness of the value of urine sampling for biomarker testing.
Also work needs to be done on the worldwide accessibility of the testing and the self-sampling method.
Speakers

Rebecca Millecamps
Marketing Manager @Fujirebio Europe
Rebecca obtained a master degree in Industrial Engineering - Biochemistry and Biotechnology at the University of Applied Science in Ghent in 1996. She mastered her molecular techniques as a scientific collaborator at the laboratory of pharmaceutical Biotechnology performing human identification using DNA profiling techniques, mainly for the department of Justice in Belgium. In 1998 she started her career at Innogenetics as a product specialist and post market surveillance coordinator. Since 2017 she is marketing manager at Fujirebio, which acquired Innogenetics in 2010. In this role, she supports Fujirebio’s automated CLEIA products, the INNO-strip-based immunoassays and molecular diagnostics with main expertise in Infectious Diseases.
References:
- Bray F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68: 394-424
- Marc Brisson et al. Impact of HPV vaccination and cervical cancer screening on cervical cancer elimination: a comparative modelling analysis in 78 low-income and lower-middle-income countries. The Lancet. Vol395, Issue 10224, P575-590, Feb 2020.
- Patti E. Gravitt et al. Looking ahead : a case for HPV testing of self-sampled vaginal specimens as a cervical cancer screening strategy. Int J Cancer. 2011 Aug 1: 129(3): 517-527.
- Arbyn M. et al. 2014. Accuracy of human papillomavirus testing on self-collected versus clinician-collected samples: a meta-analysis. Lancet Oncol. Feb;15(2):172-83.
- Xu L. et al. 2018 Clinical evaluation of INNO-LiPA HPV Genotyping Extra II using the VALGENT framework. Int J Mol Sci. 19 (9), 2704.
- Sohrabi et al. 2017. IS incidence of multiple HPV genotypes rising in genital infection? J Infect Public Health. 10(6):730-733.
- Ahmadi S. et al. 2017. Human Papillomavirus genotype distribution in cervical lesions in Zanjan, Iran. Asian Pac J Cancer Prev.18(12):3373-3377.
- O'Leary MC et al. 2011. HPV type-specific prevalence using a urine assay in unvaccinated male and female 11- to 18-year olds in Scotland. Br J Cancer. 104(7):1221-1226
- Ducancelle A. et al. 2014. Interest of human papillomavirus DNA quantification and genotyping in paired cervical and urine samples to detect cervical lesions. Arch Gynecol Obstet. 290(2):299-308
- Jannes G. et al. 2018. Evaluation of the INNO-LiPA® HPV Genotyping Extra II on UCM preserved first-void urine. Poster P10-5 presented at EUROGIN 2018 (Dec 2-5, Lissabon)
- Human papillomavirus types in 115,789 HPV-positive women: a meta-analysis from cervical infection to cancer. Peng Guan et al. Int. J. Cancer: 131, 2349-2359 (2012)
- Burroni et al. 2014. HPV prevalence in paired urine and cervical samples in woman invited for cervical cancer screening. E. J Med Vir 87:508-515
- Taylor S. et al. 2016. The incidence, clearance and persistence of non-cervical human papillomavirus infections: a systematic review of the literature. BMC Infect Dis 16:293.
- Franceschi et al Vaccine 36 (2018) 4816–4822
- David Hawkes et al. Self-collection for cervical screening programs: from research to reality. Review. Cancers. 2020, 12, 1053.
- John W. Sellors et al. Comparison of self-collected vaginal, vulvar and urine samples with physician-collected cervical samples for human papillomavirus testing to detect high-grade squamous intraepithelial lesions. CMAJ. 2000 Sep 5;163(5): 513-518.
- Reference: Bansil et al. BMC Public Health 2014, 14:596. Acceptability of self-collection sampling for HPV-DNA testing in low-resource settings: a mixed methods approach.
- Pattyn J. et al. 2019. Human papillomavirus detection in urine: Effect of first-void urine collection device and timing of collection. J Virol Meth 264:23-30.
- Pathak N. et al. 2014a. Accuracy of urinary human papillomavirus testing for presence of cervical HPV: systematic review and meta-analysis. BMJ 349, g5264
- Vorsters A. et al. 2014a. Optimization of HPV DNA detection in urine by improving collection, storage, and extraction. Eur. J. Clin. Microbiol. Infect. Dis. 33 (11):2005-2014.