The interest of SPF10 PCR-based methods for HPV DNA detection in FFPE samples
HPV and associated cancers: a global burden
The past decades, prevalence studies have been done using FFPE (Formalin-fixed-paraffin-embedded) tissue specimens to investigate HPV association with a variety of clinical conditions e.g. cervical, anogenital and head and neck cancers, or oral cavity, laryngeal carcinoma, or anal, penile, and vulvar squamous cell carcinoma. The link between cervical cancer and HPV is well-established. Since 2017, direct HPV testing is recommended in the revised WHO/IARC classification to assess a correct diagnosis of the Head and Neck Squamous Cell Carcinoma (HNSCC).1
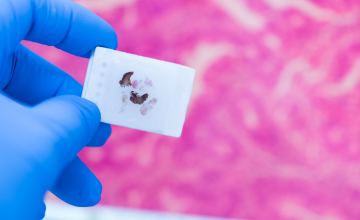
FFPE tissue: an important sample resource
FFPE tissues represent the most frequent form of tissue storage in pathology departments. These archival tissues are a potentially useful resource for epidemiological studies. Several studies have used FFPE specimens to investigate the correlation between HPV genotypes and histological classification, and/or to determine the prevalence of HPV in primary cancers.2-7
Fragmentation of DNA in FFPE samples
HPV detection and genotyping in FFPE samples is technically challenging due to poor DNA quality. Formalin fixation can cause DNA damage, including cross-linking and fragmentation.8
SPF10 PCR-based methods: most effective and most suitable
HPV DNA PCR methods amplifying shorter fragments of viral genome showed to be more sensitive and amenable for FFPE tissue. SPF10 PCR-based methods are mentioned as the most effective and most suitable for HPV DNA detection in FFPE samples because using a short HPV target region limits the risk of false-negative or invalid results.3,8-11,19
The article continues below.
INNO-LiPA HPV Genotyping Extra II on Formalin-Fixed-Paraffin-Embedded tissue
High sensitivity and specificity:
- Proven performance on cervical samples12
- The SPF10 PCR enables identification of HPV infections with low viral load and multiple HPV genotypes in one sample and one testrun12,13,14
- The small size SPF10 amplicon allows reliable amplification and accurate detection of HPV DNA also from FFPE samples5,6,14,20,21 and first-void urine15,16,17,18
- Compared to other HPV genotyping methods, INNO-LiPA is more likely to identify HPV genotypes in samples indicating low viral load and FFPE material containing multiple HPV genotypes11
Integrated controls for sample quality:
- Build-in human DNA control
- HPV control lines to confirm and detect the presence of a broad range of mucosal HPV genotypes
Prevention of co-amplification or amplicon carry-over:
- Build-in N-uracil glycosylase-based prevention minimizing the risk of PCR contamination and significantly reducing the possibility of false-positive HPV DNA results3
INNO-LiPA HPV GENOTYPING EXTRA II can play an important role in:
- Investigation of the prevalence of HPV and genotype distribution in different types of cancer 2,4-6,19-21
- Evaluation of vaccination trials and monitoring the impact of HPV vaccination (pre-and post-vaccination monitoring)15,18,19
- Epidemiological studies to investigate the prevalence and distribution of HPV types13,14
References:
- Westra W. et al. Head and neck pathology, 2017; 11:41-4
- Pretet JL. et al. Int J Cancer, 2008; 122:424-427
- Kocjan B. et al. Journal of Clinical Virology, 2016; 76:88-97S88-S97
- Sinno A. et al. Obstet Gynecol, 2014; 123:817-821
- Acuña G. et al. Modern Pathology, 2019; 32:621-626
- Fuglsang K. et al. Papillomavirus Res, 2019; 7:15-20
- Valmary-Degano S. et al. Human Pathology, 2013; 44:992-1002
- Steinau M. et al. J Mol Diagn, 2011; 13:377-381
- Tan SE. et al. J Clin Microbiol, 2010 ; 48 :1458-1460
- Querec T. et al. IPVC 2020 Book of Abstracts p.1013-1014
- Bicskei B. et al. 2020. J Cancer Sci Clin Ther, 2020; 4:349-364
- Xu L. et al. Int J Mol Sci, 2018; 19:2704
- Sohrabi A. et al. J Infect Public Health, 2017; 10:730-733
- Ahmadi S. et al. Asian Pac J Cancer Prev, 2017;18:3373-3377
- O’Leary MC. et al. Br J Cancer, 2011; 104:1221-1226
- Ducancelle A. et al. Arch Gynecol Obstet, 2014; 290:299-308
- Jannes G. et al. EUROGIN 2018 Poster P10-5
- Burroni E. et al. J Med Virol, 2015; 87:508-515
- Hillman R. et al. Int J Cancer, 2014; 135 :996-1001
- Dalla Libera LS. et al. J Oncol, 2019; Article ID 6018269
- Swangvaree SS. et al. Asian Pac J Cancer Prev, 2013; 14:1023-1026