EUROGIN 2025 – key takeaway messages
By Rebecca Millecamps, Fujirebio
The EUROGIN 2025 conference, held at the Alfândega Congress Center in Porto, Portugal, focused on advancing scientific efforts to control HPV-related cancers.
As usual, the EUROGIN program covered a wide range of topics. This summary captures the essence, highlighting the key topics and research presented.
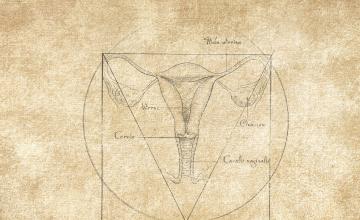
Towards more effective and efficient cervical cancer screening
Implementation of risk-stratification and self-sampling
One of the main themes was the structural and social factors impacting Human papillomavirus (HPV)-driven cancers. Discussions highlighted global inequalities in cervical cancer prevention, disparities in healthcare access, vaccination programs, and screening, particularly in low-income and marginalized communities.
Discussions at EUROGIN 2025 focused on HPV vaccination and screening in low-resource settings, presenting initiatives for cervical cancer control in underserved populations. Evidence on the high capability and cost-effectiveness of self-sampling for HPV testing, including urine sampling, was presented. Public advocacy campaigns were emphasized to improve awareness and address barriers to vaccination and screening. Updates on HPV vaccination strategies, such as single-dose and gender-neutral vaccination, were provided, along with the need to monitor impacts on existing screening programs.
Clinical validation of HPV tests is a usual key topic at the EUROGIN conference. Updates on the validation of HPV assays for primary cervical screening, including international frameworks like VALGENT and WHO guidelines were discussed.
There is a strong determination to achieve cervical cancer elimination at the European level. This commitment is reflected in almost all the European Union Member States by means of having introduced HPV vaccination and many are gradually switching to HPV detection based cervical screening. There is a strong need to update the recommendations for HPV vaccination as well as HPV detection-based screening. Future screening algorithms are envisioned to depend not only on current screening results but also on differing risk associated to previous screening participation results, biopsies and treatments, as well as vaccination uptake, risk factors exposure and demographic information. The RISCC (Risk-based Screening for Cervical Cancer Consortium) study has recently generated evidence on implementation of risk-stratified cervical screening based on HPV vaccination status. RISCC aims to improve cervical cancer screening by using risk stratification to determine who should be screened and who should be referred for colposcopy.
Use of DNA methylation markers, genotyping and self-sampling
The use of DNA methylation markers for risk stratification in cervical cancer screening was explored. Discussions underscored the potential of DNA methylation analysis to enhance cervical cancer screening and management, offering more precise and personalized approaches to prevention and care. Several studies were presented on the validation of DNA methylation markers for various clinical applications, including triage, risk stratification, and post-treatment monitoring:
- triage marker for colposcopy referral to identify women who need further examination based on their methylation profiles
- DNA methylation analysis used for risk stratification of HPV-positive women with low-grade cytology, by determining the likelihood of progression to higher-grade lesions.
- post-treatment monitoring: monitor for recurrence cervical cancer or high-grade cervical intraepithelial neoplasia (CIN2/3) and manage ongoing care.
Methylation markers are being applied to self-collected samples to triage women who test positive for HPV. This approach aims to improve the accuracy of identifying those who need further clinical follow-up. Evidence was presented on the (cost)-effectiveness of using methylation markers in self-sampling strategies, particularly in low- and middle-income countries.
The use of urine samples was discussed. This non-invasive method could potentially increase screening uptake and provide an alternative to traditional sampling methods. These samples also yielded positive results for DNA methylation analysis, allowing a full molecular workflow for screening and triage.
HPV genotyping and self-sampling are pivotal advancements in cervical cancer screening and prevention. HPV genotyping involves identifying specific HPV types present in a sample, which is crucial for understanding the risk of cervical cancer. Accurate genotyping helps in stratifying patients' risk and tailoring follow-up and treatment strategies.
Self-sampling for HPV testing is an innovative approach shown to be highly effective in increasing participation rates in cervical cancer screening programs, especially among women who might not otherwise attend regular screenings due to various barriers such as stigma, lack of access to healthcare facilities, or logistical challenges.
Recent studies have demonstrated that self-sampling is comparable to clinician-collected samples in terms of accuracy for detecting high-risk HPV types. Meta-analyses have confirmed the reliability of self-sampling, making it a viable option for large-scale implementation in screening programs.
The cost-effectiveness of self-sampling strategies has been evaluated, with findings suggesting that offering self-sampling kits can be a cost-effective way to increase screening coverage. Moreover, self-sampling has been integrated into various national screening programs, with real-world evidence supporting its effectiveness. Studies in Australia, Norway, Denmark, US and the Netherlands have shown successful implementation of self-sampling, leading to increased screening uptake and early detection of HPV-related lesions.
In addition to increasing screening participation, self-sampling can be used also to triage HPV-positive women using DNA methylation markers and/or extended HPV genotyping. These approaches help ensure that women with underlying lesions are accurately identified and managed accordingly.
HPV genotyping, DNA methylation and self-sampling represent significant advancements in cervical cancer prevention. They offer a promising solution to increase screening coverage, improve early detection, and ultimately reduce the incidence and mortality of cervical cancer. As research continues to evolve, these methods are expected to play an increasingly important role in global cervical cancer control efforts.
Artificial intelligence (AI)
The growing role of AI data analysis in HPV-related cancers was explored, with discussions on AI applications in cancer screening, diagnosis, and management, including machine learning models for predicting cancer progression.
Other HPV-related cancers
Guidelines for anal cancer screening have recently been published in several countries. A broad review of those recommendations was presented, addressing populations targeted for screening, country specific differences in the guidelines, and the accuracy of different biomarkers.
Updates on anogenital carcinogenesis were provided. Biomarkers for anal cancer screening, including DNA methylation, and the clinical characteristics of HPV-related gynaecological diseases were examined.
The conference also covered advances in the epidemiology, prevention, and treatment of HPV-related head and neck cancers, including the role of liquid biopsies and personalized therapy.
Accelerating universal and gender-neutral HPV vaccination was discussed, as a tool to move more rapidly towards the goal of cancer elimination while providing protection against HPV-related diseases for both females and males.
The EUROGIN 2025 conference underscored significant advancements in HPV-related cancer prevention and screening, emphasizing the importance of universal and gender-neutral vaccination, and innovative approaches such as self-sampling, DNA methylation markers, genotyping, and AI applications. These developments pave the way for more effective and equitable healthcare solutions, promising a brighter future in the fight against HPV-related cancers.