Cervical cancer screening being reviewed – the role of distinguishing individual HPV genotypes
By Rebecca Millecamps, Fujirebio
The article below is part of a series of resources dedicated to the state-of-the-art of HPV testing.
Get a full overview of our resources here.
Screening guidelines and new technologies are being reviewed
Cervical screening guidelines are being reviewed and changed in response to new evidence as it becomes available. At EU level the cancer screening guidelines were updated in 2015 with recommendation for population-based screening programs and introduction of human papillomavirus (HPV) testing starting at the age of 30 with a five-year interval. Following these EU guidelines France, Germany, Italy, Spain, Sweden have recently updated their guidelines.1 Belgium recently announced to introduce HPV-based screening by 2024.
New technologies for screening and triage are being evaluated and algorithms are being compared. HPV- and cytology-based cervical screening clearly show an established reduction in cervical cancer incidence and mortality but what about benefit-to-harm balance? Comparing HPV DNA vs cytology or HPV DNA vs co-testing shows that HPV DNA primary testing offers the best benefit-to-harm balance.2
A necessary next step is to reduce the referral rates for follow-up and/or treatment with an improved triage of hrHPV-positive women. Stratifying risk groups is key to implement a highly effective strategy which avoids unnecessary pelvic exams and colposcopy services being overwhelmed with referrals of women who have in majority of the cases a low risk of pre-invasive or invasive disease.
HPV genotyping information could enable optimized clinical management of screened women depending on the oncogenic risk associated with the different genotypes.3
The article continues below.
Improved risk stratification with HPV16/18 genotype information
As HPV-based primary screening programmes around the world evolve and are adapted to the latest evidence, partial genotyping is expected to increasingly find its place as a key strategy for maximising the benefits, and minimising the harms, of cervical screening.4
Among HPV-positive women, HPV genotyping can be used in addition to cytology to effectively stratify the risk of precancer. In the 2012 American Society for Colposcopy and Cervical Pathology (ASCCP) guidelines and 2015 ASCCP clinical guidance, partial genotyping was incorporated into management; women with HPV-positive, cytology of Negative for Intraepithelial Lesions or Malignancy (NILM) were referred to colposcopy if the highest-risk HPV types (HPV16 or HPV18) were detected. 5 The 2019 guidelines further align management recommendations with current understanding of HPV natural history and cervical carcinogenesis with a change from primarily test results-based algorithms to primarily “risk-based” guidelines.6
The Netherlands, as one of the first countries introducing HPV-based primary screening, updated their screening algorithm in July 2022 by implementing HPV16 and HPV18 genotype information combined with cytology assessment for either direct referral to colposcopy (HPV16/18 positive and ≥ASCUS) or retest in 6 months if HPV16/18 negative and NILM.7
In a Norwegian pilot, triage of high-risk human papillomavirus (hrHPV)-positive women with reflex cytology followed by hrHPV testing 12 months later, yielded 82% of women referred to colposcopy (hrHPV and reflex cytology positive or hrHPV positive at 12 months follow-up) and 24% with cervical intraepithelial neoplasia grade 3 or worse (CIN3+). A policy stratified by the presence of HPV16/18 would be more efficient (66% referred to colposcopy) at the expense of small losses in the detection of precancer.4
Partial genotyping-based colposcopy referral strategies can be explicitly designed to take into account the rapidly dropping prevalence of HPV16/18 in young women due to population-level impact of HPV vaccines. Such an approach is already being used in Australia where HPV16/18 rates are now +/-2% or less, enabling the practical implementation of HPV screening and immediate colposcopy referral for all HPV16/18-positive women from the age of 25 years, whereas women with other hrHPV infections are triaged with cytology.4
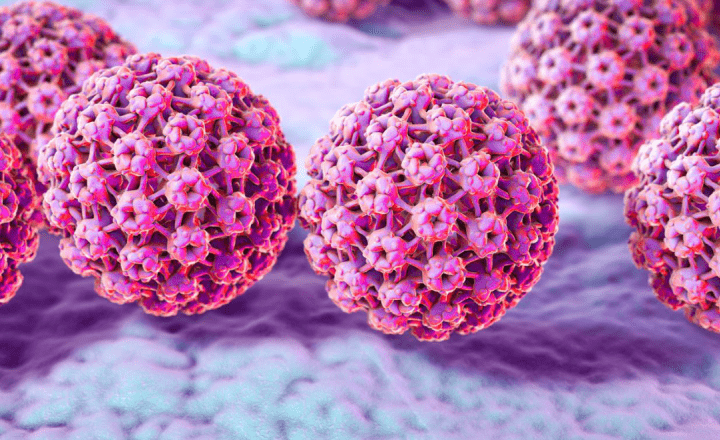
Risk progression differs substantially by HPV genotype
Extended genotyping methods have not been studied as extensively as partial genotyping for immediate triage of hrHPV-positive women.
Risk of progression differs substantially by HPV type and regrouping of hrHPV genotypes based on carcinogenicity is being discussed and thoroughly studied. A more complete differentiation between genotypes may improve triage of low-grade intraepithelial lesion (LSIL) cytology. The concept of grouping genotypes into bands, tiers, or clusters may ease the implementation of genotype information into screening algorithms as it simplifies the clinical management. Genotype information can be used as a triage method for HPV-positive women, reducing the cost of traditional colposcopy-based confirmation. However, formal evaluation and recommendations by groups issuing clinical testing guidelines is needed to enable large-scale implementation.8,9
Combining existing and available methods could offer the most optimal triage strategy
Although HPV genotyping is currently already an accepted triage test in some countries, it is important to stay alert and evaluate possible implications for screening and management when using (extended) HPV genotyping in screening and triage settings, taking into account also vaccinated populations that are now entering the screening age range. Partial HPV genotyping would be a suitable triage option for populations where vaccination coverage is still below an acceptable threshold (such as less than 80%) for an effect in preventing CIN2+. In the unvaccinated population partial genotyping appears more sensitive than cytology.9
HPV genotyping clearly provides good risk-stratification but it doesn’t distinguish between transient infections and those that are most likely to progress to cervical cancer.
DNA methylation of viral and/or host cell genes are identified as promising tools to identify HPV positive women with cervical precancer and cancer in several studies.10,11
Methylation, in combination with cytology or HPV genotyping, can be used to support a wait-and-see policy in women with CIN2/3. A combined HPV16 and methylation testing identifies a subgroup with a high clinical regression rate.10
The discriminative power of FAM19A4/miR124-2 methylation, HPV16/18 genotyping and HPV16/18/31/33/45 genotyping in HPV positive women with ASC-US/LSIL cytology triage test has been evaluated in Dutch screening trials. The CIN3+ risk after a negative result could be lowered by combining methylation and extended genotyping, at the expense of a higher referral percentage. The use of FAM19A4/miR124-2 methylation and/or HPV genotyping in HPV-positive women with borderline or mild dyskaryosis cytology (ASC-US/LSIL) can lead to a substantial reduction in the number of direct colposcopy referrals.11
No one-size-fits-all solution yet
Combining existing and available methods could offer the most optimal triage strategy.
There is a growing menu of useful and well-validated technologies for cervical cancer screening, triage and management offering different choices or possibilities to accommodate different country- or population specific needs.
References
- Wang W. et al. Prev Med Rep. 2022 May 8;28:101813.
- Bouvard NEJM 2021 Nov.11:385(20):1908-1918.
- Liverani CA et al. J Oncol. 2020 Nov 5;2020:8887672.
- Marc Arbyn et al. British Journal of Cancer (2020) 122:1577–1579.
- Demarco M. et al. J Low Genit Tract Dis. 2020 Apr;24(2) :144-147.
- Perkins RB et al. J Low Genit Tract Dis. 2020 Apr;24(2):102-131.
- https://www.rivm.nl/bevolkingsonderzoek-baarmoederhalskanker/professionals/hoe-verloopt-screening/verwijsschema
- Bonde J. et al. Journal of Lower Genital Tract Disease 2020 Jan;24(1):1-13.
- Leeson S. et al. Eur J Obstetrics & Gynecology and Reproductive Biology 2021;258:332-342.
- Wieke W. Kremer et al. J Clin Oncology 2022.
- Dick S. et al. Br J Cancer 2022 126, 259–264.