Improved triage with FAM19A4/miR124-2 methylation analysis - clinical assurance thanks to objective and reliable results
By Rebecca Millecamps, Fujirebio
The article below is part of a series of resources dedicated to the state-of-the-art of HPV testing.
Get a full overview of our resources here.
Transition towards high-risk human papillomavirus (hrHPV) testing as primary screening
hrHPV testing is replacing cytology as primary screening method for cervical cancer screening in an increasing number of countries. Advantages of primary hrHPV testing are the objectivity of the assay and high-throughput testing, and its high sensitivity of 90% for CIN2 or worse (≥CIN2) and 95% for CIN3 or worse (≥CIN3), compared to moderate sensitivity of 30–87% for cytology. Four European prospective randomised screening studies have shown a 60-70% reduction in cervical cancer rates for those with negative tests including adenocarcinoma.1
Need for improved triage of hrHPV positive women
On the other hand, the major limitation of hrHPV testing is its inability to distinguish transient infections from clinically relevant infections, resulting in reduced specificity compared to cytology. This results in higher numbers of unnecessary colposcopy referrals compared to cytology screening, as has been observed in the Netherlands (increase from 2.5% to 4.2%). Also, observational studies from England and Finland report an increase in referral rates of 53% and 98%, respectively.2
Management of hrHPV positive women and the most preferable triage method or strategy is a topic of discussion today. There is currently no international consensus on criteria for triage strategies.
General requirements for triage methods
In general, the aspects listed below are required for triage tests within cervical screening programs. The optimal balance between these requirements varies between regions, depending on locally accepted risk thresholds, available resources and population characteristics3,4:
- High sensitivity
- High Negative Predictive Value (NPV) for CIN3+ and cervical cancer offering assurance for absence of cervical cancer in case of negative result.
- High specificity
- High Positive Predictive Value (PPV) of at least 20% (the Netherlands) or 5-10% (USA) to ensure women who test positive are accurately targeted for management, avoiding overtreatment, associated cost and patient anxiety.
- Long term safety demonstrated by means of longitudinal studies evaluating the long-term CIN3+ and cervical cancer risk of triage negative women, to determine appropriate screening intervals with chosen triage strategy.
- High reproducibility
- No need for additional sample or additional visit to perform triage testing, thus minimizing the efforts for the screened women, and to limit loss to follow-up.
The article continues below.
A variety of tests are being evaluated
A variety of tests are now available to distinguish hrHPV positive women who need immediate referral to colposcopy from those who need early repeat HPV test or recall based on their disease status. Different methods, e.g. partial genotyping, dual staining, HPV E6/E7 mRNA and DNA methylation, are being evaluated as single options or as combined algorithms, considering also cost effectiveness.4,5,6
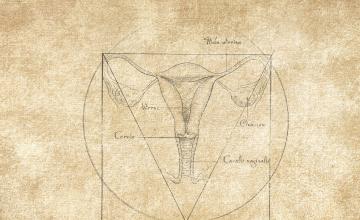
The worldwide experience with cytological assessment of cervical samples makes cytology an interesting triage method for hrHPV-positive women; however, limitations as average sensitivity, subjectivity of the analysis, and inability to perform on self-sampled material are major disadvantages. To improve sensitivity, different immunochemistry stains, as p16 staining, or p16/Ki-67 dual-stain can be used as biomarker. However, these triage strategies are still more or less based on morphological criteria and cannot differentiate between productive and transforming infections or predict the development of high-grade lesions. Besides, they are not applicable on self-sampled specimens, which may play an important future role in hrHPV-based screening. An additional clinician-taken sample would still be needed for further triage of hrHPV-positive women.3
A combination triage involving any of two of cytology, HPV partial genotyping or dual-staining seems most efficient at present. However, HPV vaccination may impact the performance of future partial genotyping.5
DNA methylation is easily detectable in clinician-taken, self-sampled, and histological cervical specimens. Understanding the role of epigenetic events in host and viral genes is an important and promising area of investigation and is expected to result in novel risk stratifying strategies for triage of hrHPV-positive women. Methylation markers based on host DNA methylation have been studied extensively and have been summarized in reviews indicating a promising role in triage of hrHPV-positive women. Several markers and combinations of markers have been studied widely, including miR-124-2 and FAM19A4 showing promising results.3
Increasing knowledge on molecular markers - FAM19A4/miR124-2 methylation analysis
High sensitivity and high specificity
FAM19A4/miR124-2 methylation analysis shows a high sensitivity for cervical cancer (95.0-100.0%) and CIN3+ (78.6%), combined with a high specificity for CIN3+ (76.8%).7,8
High Negative and Positive Predictive Value
The high sensitivity and consequently a high Negative Predictive Value (NPV) of 96.9% for CIN3+ offers assurance for absence of cervical cancer in case of a negative FAM19A4/miR124-2 methylation result. The high specificity and consequently high Positive Predictive Value (PPV) for CIN3+ of 28.3% as colposcopy triage test of HPV-positive women exceeds the PPV threshold for colposcopy referral in the US (10%) and may other western countries (10-20%).10 It offers assurance that women are identified who are actually in need for immediate treatment.
Longitudinal data – long term safety in population-based screening program
There are few prospective studies evaluating DNA methylation markers to conclusively assess their potential as predictors of future or progressing cervical lesions. Longitudinal evaluations to measure safety of triage strategies are needed. For the FAM19A4/miR124-2 methylation test however, a longitudinal study among 1040 HPV-positive women with a 14-year follow-up period reported that, compared to a cytology negative (<ASCUS) result at enrolment, a negative FAM19A4/miR124-2 methylation test indicated lower risk of cervical cancer incidence and a similar risk for CIN3+, over a 14- year follow-up period.9 A similar longitudinal study was done to evaluate the cervical cancer risk in HPV-positive women after a negative FAM19A4/miR124-2 methylation test, showing that this methylation test provides a low cervical cancer risk in hrHPV-positive women of 1.7%, which is even lower than the risk with a negative cytology result (2.4%).10 The major strengths of these studies are the setting within a population-based screening program, its large sample size, the long follow-up period (14 years) and the wide age range (29-61 years).9,10
Self-samples
Performance of the FAM19A4/miR124-2 methylation analysis has also been evaluated with lavage- and brush-based self-samples, resulting in a ≥ CIN3 sensitivity of 70.5% and 69.4% with a specificity of 67.8 and 76.4% respectively.13
Prognostic value
Several biomarkers have been evaluated for their prognostic value such as HPV viral load and immunohistochemical staining of p16INK4A and Ki-67, but none of these were able to predict regression or progression of CIN. Studies have shown that DNA methylation levels of host cell genes and viral genes increases with severity of CIN grade and are very high in cervical cancer. Recent studies showed that a FAM19A4/miR124-2 methylation analysis identifies CIN2/CIN3 lesions at the highest short-term risk of progression to cervical cancer (requiring treatment) and predicts regression allowing a wait-and-see policy (follow-up).11,12
Combined strategies to increase clinical value
Combining host methylation markers and HPV genotyping may increase the clinical value versus using both these methods separately for triage of hrHPV-positive women. Combined HPV genotyping and methylation testing in women with an HPV-positive cervical sample showed a high regression incidence of 85.1% after a double negative result and a substantially lower regression incidence of 44.7% after a double-positive result. Clinical regression reached an intermediate level of 56.9% after an HPV16-positive/methylation-negative result and 61.9% after an HPV16-negative/methylation-positive result.11
FAM19A4/miR124-2 methylation analysis could be the key to full molecular screening
All these studies demonstrate FAM19A4/miR124-2 methylation can be considered as an alternative to cytology as follow-up test for hrHPV positive women given its performance combined with the added advantages of objectivity, automation and use of self-collected samples. It could be the key to full molecular screening, incorporating even a predictive value.4,7,9,10,11,13
References:
- Ronco G. et al., Lancet 2014;383(9916):524-532.
- Loopik DL, et al. Am J Obstet Gynecol 2021;224:200
- Renée MF Ebisch, et al. Expert Review of Anticancer Therapy 2016;16(10):1073-1085
- Kelly H. et al., Br J Cancer. 2019 Nov;121(11):954-965
- Leeson S., et al. Eur J Obs & Gynecology and Reproductive Biology 258 (2021) 332-342
- Onyango CG et al., Infect Agent Cancer. 2020 Nov 16;15(1):68
- Bonde J., et al. Int. J. Cancer. 2021;148(2):396-405
- Vink F.J., et al. Int J Cancer. 2020; 147:1215-1221
- Dick S., et al. Gynecol Oncol. 2019;154(2):368-373
- De Strooper L.M., et al. Int. J. Cancer. 2018;143(6):1541-1548.
- Kremer W.W., et al. J Clin Oncol. 2022;40(26):3037-3046
- Vink F.J., et al. Int. J. Cancer. 2021;149:707-716.
- De Strooper LM, et al. Gynecol Oncol. 2016;141(2):341–347