The drawbacks of relying solely on the standard routine clinical examinations and cognitive testing
By Rianne Esquivel and Dr. Nathalie Le Bastard, Fujirebio
- You can download this entire article as a PDF here (Premium eServices resource)
Many subtypes of disease exist under the umbrella of dementia with Alzheimer’s disease (AD) being the most common. AD-related dementia is characterized by neuropathological changes in the brain.
Amyloid plaques and tangles made of hyperphosphorylated tau build up in the brain and are hallmarks of the disease. The presence of these neuropathological changes is necessary for a true AD diagnosis.
Because of this requirement, the true gold standard for AD diagnosis can only occur upon autopsy.
Currently, differential diagnosis is used to assess early onset of dementia for the millions of patients suffering from early symptoms of memory loss and cognitive complaints.
Thus, for the last 45 years clinicians have relied primarily on a cognitive assessment including cognitive screening tests such as the Mini-Mental State Examination (MMSE) and more recently the Montreal Cognitive Assessment (MoCA), alongside a clinical workup to diagnose AD (Dubois et al., 2021).
The MMSE is a paper-based test that has long been used as part of the process when considering a diagnosis of dementia, whereas the MoCA was developed as a tool to screen patients who present with mild cognitive complaints and usually perform in the normal range on the MMSE (Creavin et al., 2016; Nasreddine et al., 2005).
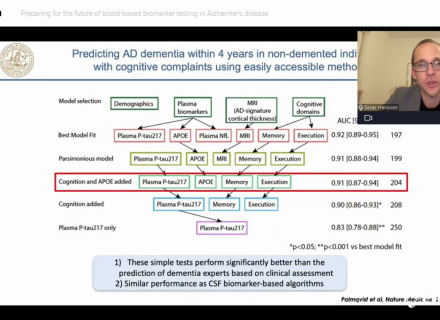
While clinical diagnosis relying primarily on cognitive tests can reach 70% to 90% accuracy in late stages of AD, it is much less accurate in early stages of mild cognitive impairment (MCI) due to AD, and it is well known that MCI can have many pathological causes unrelated to AD (Breton et al., 2019; Schneider et al., 2009).
Additionally, differentiating AD from non-Alzheimer’s (non-AD)-related dementias is challenging with cognitive screening tests alone.
The inaccuracy of clinical diagnosis utilizing only cognitive tests to diagnose early AD has been observed by comparing neuropathological results after autopsy.
In a longitudinal community-based clinical-pathologic study, 483 older persons underwent a battery of cognitive tests including the MMSE. Of the 179 persons diagnosed with probable AD, 88% were confirmed to have AD by pathologic criteria. However, when examining the 134 persons with MCI, the number of patients with pathologically confirmed AD was reduced to 54% of which 59% had amnestic MCI and 49% non-amnestic MCI; despite that amnestic MCI is often thought to be a more specific sign of early AD (Salmon, 2011; Schneider et al., 2009).
This indicates that symptommatology and cognitive tests alone cannot be used to reliably diagnose early AD.
As clinical diagnosis improves further along the AD spectrum, longitudinal analysis may be used to determine whether MMSE scores accurately predict conversion to AD dementia from MCI. While this is not the intended use of cognitive tests, that is what they are tasked with if used to diagnose AD at the MCI stage.
A systematic review of eight studies spanning 1128 patients looked at whether MMSE scores accurately predicted MCI conversion to AD. The review found highly variable outcomes in sensitivity and specificity, ranging from 27% to 89% and from 32% to 90% respectively. Pooling these studies at a median specificity of 80%, resulted in a sensitivity of 54%.
Thus, in a hypothetical cohort of 100 MCI patients with a 39.2% incidence of AD, the number of missed cases would be 18 patients and 12 MCI patients would be over diagnosed. The review did not find evidence supporting a substantial role of MMSE as a stand-alone single-administration test in the identification of MCI patients who may develop dementia (Arevalo-Rodriguez et al., 2015).
While many studies have determined that the MoCA has higher diagnostic accuracy for MCI than the MMSE, to our knowledge none have looked at the MoCA in relation to AD pathology in MCI (Breton et al., 2019).
Thus, it is important to clarify, while the MoCA may have high sensitivity for distinguishing MCI from AD or healthy controls it has not been validated for determining the underlying pathology of MCI.
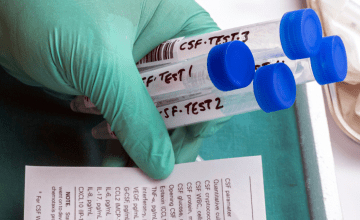
In more recent years, amyloid PET (positron emission tomography) and cerebrospinal fluid (CSF) testing have emerged as important tools to determine the presence of amyloid pathology. Amyloid PET is used to estimate β-amyloid neuritic plaque density in adult patients’ brains with cognitive impairment who are being evaluated for AD and other causes of cognitive decline.
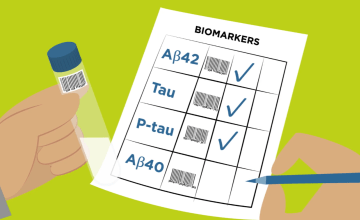
CSF biomarker testing utilizes four core biomarkers; 2 β-amyloid biomarkers (Aβ1-42 and Aβ1-40 as part of the Aβ1-42/Aβ1-40 ratio), and 2 Tau biomarkers (pTau and tTau) to determine amyloid status and the presence of other AD-related pathological changes.
In the next chapter we will review available literature on the accuracy of the underlying pathological determinations in MCI and non-AD patients during clinical diagnosis and how PET and CSF testing can influence an accurate amyloid status determination.
The importance of correctly identifying the neurobiological cause of the dementia is critical when considering which patients to enroll in clinical trials to develop novel therapies and which patients will benefit from amyloid and tau targeted therapies.
As current therapies focus on preventing cognitive decline and treating symptoms rather than a cure, it is critical to determine amyloid pathology early in the AD spectrum at the MCI stage.
For those patients who do not have AD dementia, it is critical to avoid unwanted side effects from mistargeted drugs as well as to gain access to treatments that may be warranted for other causes of cognitive decline.
References
- Arevalo-Rodriguez, I., Smailagic, N., Roquéi Figuls, M., Ciapponi, A., Sanchez-Perez, E., Giannakou, A., Pedraza, O. L., Bonfill Cosp, X., & Cullum, S. (2015). Mini-Mental State Examination (MMSE) for the detection of Alzheimer’s disease and other dementias in people with mild cognitive impairment (MCI). In Cochrane Database Syst Rev, 7(7):CD010783. https://doi.org/10.1002/14651858.CD010783.pub2
- Breton, A., Casey, D., & Arnaoutoglou, N. A. (2019). Cognitive tests for the detection of mild cognitive impairment (MCI), the prodromal stage of dementia: Meta-analysis of diagnostic accuracy studies. Int J Geriatr Psych, 34(2):233-242. https://doi.org/10.1002/gps.5016
- Creavin, S. T., Wisniewski, S., Noel-Storr, A. H., Trevelyan, C. M., Hampton, T., Rayment, D., Thom, V. M., Nash, K. J. E., Elhamoui, H., Milligan, R., Patel, A. S., Tsivos, D. v., Wing, T., Phillips, E., Kellman, S. M., Shackleton, H. L., Singleton, G. F., Neale, B. E., Watton, M. E., & Cullum, S. (2016). Mini-Mental State Examination (MMSE) for the detection of dementia in clinically unevaluated people aged 65 and over in community and primary care populations. Cochrane Database Syst Rev (1):CD011145. https://doi.org/10.1002/14651858.CD011145.pub2
- Dubois, B., Villain, N., Frisoni, G. B., Rabinovici, G. D., Sabbagh, M., Cappa, S., Bejanin, A., Bombois, S., Epelbaum, S., Teichmann, M., Habert, M. O., Nordberg, A., Blennow, K., Galasko, D., Stern, Y., Rowe, C. C., Salloway, S., Schneider, L. S., Cummings, J. L., & Feldman, H. H. (2021). Clinical diagnosis of Alzheimer’s disease: recommendations of the International Working Group. Lancet Neurol, 20(6):484-496. https://doi.org/10.1016/S1474-4422(21)00066-1
- Nasreddine, Z. S., Phillips, N. A., Bédirian, V., Charbonneau, S., Whitehead, V., Collin, I., Cummings, J. L., & Chertkow, H. (2005). The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J Am Geriatr Soc, 53(4):695-699. https://doi.org/10.1111/j.1532-5415.2005.53221.x
- Salmon, D. P. (2011). Neuropsychological features of mild cognitive impairment and preclinical alzheimer’s disease. Curr Top Behav Neurosci, 10:187-212. https://doi.org/10.1007/7854_2011_171
- Schneider, J. A., Arvanitakis, Z., Leurgans, S. E., & Bennett, D. A. (2009). The neuropathology of probable Alzheimer disease and mild cognitive impairment. Ann Neurol, 66(2):200-208. https://doi.org/10.1002/ana.21706