On November 3, 1906, the German clinical psychiatrist and neuroanatomist Alois Alzheimer reported “A...
When To Use Blood-Based Biomarkers For Alzheimer's Disease Assessment
Nov 19, 2025
Accelerating Alzheimer’s diagnosis with blood-based biomarker testing
Studies indicate that patients may wait an average of more than three years for an accurate diagnosis of Alzheimer's disease (AD).1 Such delays can limite timely access to recently approved disease-modifying therapies for early Alzheimer’s disease, defined as mild cognitive impairment (MCI) or mild dementia due to AD. 2,3 Blood-based biomarker testing, which is less invasive and more accessible than amyloid positron emission tomography (PET) imaging or cerebrospinal fluid (CSF) testing, has demonstrated robust clinical performance and has the potential to significantly shorten this diagnostic timeline.4
When to order a blood test
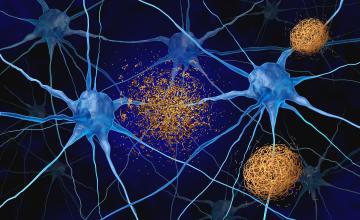
Blood-based biomarker tests are designed to detect beta-amyloid (Aβ) pathology in the brain, a hallmark of Alzheimer’s disease. Since currently approved disease-modifying therapies are indicated only for symptomatic individuals—and because these tests have not yet been validated in asymptomatic patients, recent clinical recommendations and consensus frameworks advise their use only in patients with documented cognitive impairment. 5,6
Depending on their performance characteristics, these blood-based biomarker tests can serve different roles in the diagnostic pathway. Triage tests are designed to have high sensitivity, helping clinicians rule out Alzheimer's disease pathology and reduce unnecessary CSF or PET testing but sacrifice specificity. Confirmatory tests have high specificity, providing sufficient accuracy to confirm the presence of amyloid pathology and potentially replace CSF tests and amyloid PET imaging in the diagnostic workup.
Guidelines for choosing a reliable blood test
Recently, the Alzheimer’s Association published clinical practice guidelines for the use of blood-based biomarkers, and the Global CEO Initiative (CEOi) on Alzheimer’s Disease released a consensus framework outlining performance and implementation standards for these tests .5,6 Together, these efforts provide guidance on appropriate clinical use, result interpretation, and the performance thresholds needed to ensure reliable patient care decisions.
While the Alzheimer’s Association clinical practice guidelines specify performance thresholds using only sensitivity and specificity, the CEOi recommendations include these same parameters and additionally provide metrics for negative and positive predictive values (NPV and PPV) based on pre-test probability.
- Alzheimer’s Association clinical practice guidelines:
- Recommended the use of blood-based biomarker tests in specialized memory-care settings, rather than in primary care.
- Triage testing:
- ≥90% sensitivity and ≥75% specificity. 5
- Confirmatory testing:
- ≥90% sensitivity and ≥90% specificity. 5
- CEOi recommendations:
- Provided performance metrics for both primary and specialty care settings
- Triage testing:
- Primary care (20% prevalence of amyloid pathology): ≥90% sensitivity and ≥85% specificity, expected PPV of 60% and NPV of 97%6
- Specialty care (50% prevalence of amyloid pathology): ≥90% sensitivity and ≥85% specificity, expected PPV of 86% and NPV of 89%6
- Confirmatory testing (both primary and specialty care):
- Primary care (20% prevalence of amyloid pathology): ≥90% sensitivity and ≥90% specificity, expected PPV of 69% and NPV of 97% 6
- Specialty care (50% prevalence of amyloid pathology): ≥90% sensitivity and ≥90% specificity, expected PPV of 90% and NPV of 90%6
- Performance data for individual tests are compiled in the CEOi Alzheimer’s Blood Test Performance Database.7
Fujirebio’s FDA-cleared blood test for the assessment of Alzheimer's disease
On May 16, 2025, the FDA cleared the first blood-based in vitro diagnostic (IVD) test for the assessment of Alzheimer’s disease: the Lumipulse® G pTau 217/β-Amyloid 1-42 Plasma Ratio. This test is indicated for adult patients, aged 50 years and older, presenting at a specialized care setting with signs and symptoms of cognitive decline.8
This test measures two Alzheimer’s disease-related protein biomarkers in plasma:
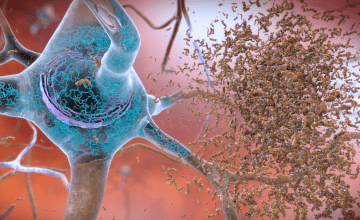
- pTau 217: A tau protein phosphorylated at threonine 217, elevated in individuals with β-amyloid pathology,9
- β-Amyloid 1-42: A peptide that aggregates into amyloid plaques. Lower plasma levels are associated with β-amyloid pathology.10
The concentrations of these biomarkers are combined into a numerical ratio (pTau 217/β-
Amyloid 1-42) and reported as quantitative values. Results are interpreted using two predefined cutpoints that divide results into three categories:8,11
- Negative (≤0.00370): Consistent with patients who are unlikely to have amyloid pathology. These patients should be investigated for other potential causes of cognitive decline.
- Indeterminate (0.00371–0.00737): Consistent with patients for whom amyloid pathology is uncertain. These patients should be considered for further testing.
- Positive (≥0.00738): Consistent with patients who are likely to have amyloid pathology. This result does not establish a diagnosis of AD or other cognitive disorders.
In a clinical study of 499 patients that included individuals with subjective cognitive decline (SCD), mild cognitive impairment (MCI), AD, and other neurodegenerative conditions, the Lumipulse® G pTau 217/β-Amyloid 1-42 Plasma Ratio test demonstrated 97.6% sensitivity and 90.8% specificity when compared with amyloid PET and CSF test results7. In this cohort, which had an observed amyloid pathology prevalence of 51%, these values corresponded to a PPV of 92% and an NPV of 97%, with 19.6% of patients receiving an indeterminate result.11.
When examined by clinical diagnostic category, the test also performed well across the early AD continuum. 11 Among patients with MCI, the PPV was 90% and the NPV was 98.6%. In those with SCD, PPV and NPV were 92% and 100%, respectively. 11 These findings highlight the potential clinical value of the test to detect early-stage disease when diagnostic certainty and timely therapeutic intervention are most critical.
Together, recent clinical practice guidelines and performance recommendations for blood-based biomarkers, along with FDA-cleared diagnostic tools like the Lumipulse® G pTau 217/β-Amyloid 1-42 Plasma Ratio test, are advancing the clinical assessment of Alzheimer’s disease. By enabling accurate detection of amyloid pathology through a simple blood draw, these developments support earlier intervention, more informed care decisions, and improved access to disease-modifying therapies.
For additional details, please consult the Blood-Based Biomarker Learning Guide.
References:
- Kusoro O, Roche M, Del-Pino-Casado R, Leung P, Orgeta V. Time to Diagnosis in Dementia: A Systematic Review With Meta-Analysis. Int J Geriatr Psychiatry. 2025;40(7). doi:10.1002/gps.70129
- van Dyck CH, Swanson CJ, Aisen P, et al. Lecanemab in Early Alzheimer’s Disease. New England Journal of Medicine. 2023;388(1):9-21. doi:10.1056/NEJMoa2212948
- Sims JR, Zimmer JA, Evans CD, et al. Donanemab in Early Symptomatic Alzheimer Disease. JAMA. 2023;330(6):512. doi:10.1001/jama.2023.13239
- Mattke S, Chen J, Hanson M. Impact of a High-Performing Blood Test on Wait Times for Determination of Eligibility for a Disease-Modifying Alzheimer’s Treatment in the U.S. Alzheimer’s & Dementia. 2024;20(S7). doi:10.1002/alz.091612
- Palmqvist S, Whitson HE, Allen LA, et al. Alzheimer’s Association Clinical Practice Guideline on the use of blood-based biomarkers in the diagnostic workup of suspected Alzheimer’s disease within specialized care settings. Alzheimer’s & Dementia. 2025;21(7). doi:10.1002/alz.70535
- Schindler SE, Galasko D, Pereira AC, et al. Acceptable performance of blood biomarker tests of amyloid pathology — recommendations from the Global CEO Initiative on Alzheimer’s Disease. Nat Rev Neurol. 2024;20(7):426-439. doi:10.1038/s41582-024-00977-5
- Global CEO initiative on Alzheimer’s disease. The CEOi Alzheimer’s Blood Test Performance Database. Alz Biomarker Hub. Accessed July 8,
- 2025. https://www.alzbiomarkerhub.org/performance-database-tool
- Fujirebio Receives Marketing Clearance for Lumipulse® G pTau 217/β-Amyloid 1-42 Plasma Ratio In-Vitro Diagnostic Test As An Aid To Identify Patients With Amyloid Pathology Associated With Alzheimer’s Disease. Fujirebio. 2025. Accessed July 1, 2025. https://www.fujirebio.com/en-us/news-events/fujirebio-receives-marketing-clearance-for-lumipulser-g-ptau-217bamyloid-142-plasma-0
- Mattsson-Carlgren N, Janelidze S, Palmqvist S, et al. Longitudinal plasma p-tau217 is increased in early stages of Alzheimer’s disease. Brain. 2020;143(11):3234-3241. doi:10.1093/brain/awaa286
- Lopez OL, Klunk WE, Mathis CA, et al. Relationship of amyloid-β1–42 in blood and brain amyloid: Ginkgo Evaluation of Memory Study. Brain Commun. 2020;2(1). doi:10.1093/braincomms/fcz038
- U.S. Food and Drug Administration. (2025, May 16). Lumipulse G pTau 217/β-Amyloid 1-42 Plasma Ratio: 510(k) decision summary (K242706).
- https://www.accessdata.fda.gov/cdrh_docs/pdf24/K242706.pdf