On November 3, 1906, the German clinical psychiatrist and neuroanatomist Alois Alzheimer reported “A...
Modern Alzheimer’s Diagnosis: What Clinicians Need to Know About Biomarkers and Staging
May 8, 2025
What PET scans, CSF assays, and blood tests reveal about Alzheimer’s — and how the A/T/N framework supports earlier, more accurate diagnoses.
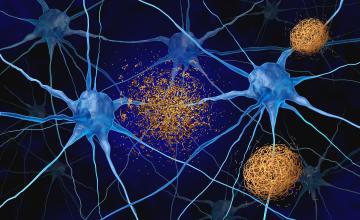
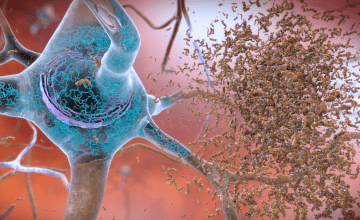
Alzheimer’s disease diagnosis is evolving. For most of modern medical history, confirming an Alzheimer’s disease diagnosis required a post-mortem brain examination to detect the disease’s hallmark pathologies: beta-amyloid plaques, tau tangles, and neurodegeneration. But in recent decades, advances in imaging and fluid biomarkers have enabled clinicians to detect these changes in living individuals — often years before clinical symptoms appear.
In 2016, researchers involved with the Alzheimer’s Association Working Group introduced the A/T/N classification framework, as a biomarker-based system to standardize the assessment of pathology.1 This framework marked a shift away from a symptom-based diagnosis — to a biological definition of Alzheimer’s disease, applicable across the entire disease continuum.
Since then, the guidelines have continued to evolve. The recently published revised criteria for the diagnosis and staging of Alzheimer’s disease introduced blood-based biomarker tests and broadened the scope of detectable disease processes.2
What is A/T/N?
The A/T/N framework categorizes biomarkers into three groups based on the specific aspect of Alzheimer’s disease pathophysiology they reflect, with each corresponding to a core pathological process:
- A (Amyloid): indicators of beta-amyloid plaque build-up
- T (Tau): markers of aggregated tau proteins, forming neurofibrillary tangles
- N (Neurodegeneration): signs of neuronal injury or loss
Each category is assessed using a binary classification system, meaning each marker is labeled as either positive (+) or negative (-), creating a standardized way to describe a person’s biomarker profile. For instance, an A+/T+/N- result indicates the presence of amyloid and tau pathology in the absence of measurable neurodegeneration. This binary classification helps determine whether changes are consistent with Alzheimer’s disease pathology, even in early or atypical cases. Originally developed for research, the framework was designed to define Alzheimer’s disease biologically — independent of clinical symptoms.
Beyond A/T/N: Core Biomarkers and Emerging Pathophysiological Markers
While the original A/T/N framework was developed primarily for research purposes, the revised criteria build upon it to support use in clinical contexts.2 At the center of the revised criteria approach is the categorization of biomarkers into core and non-core groups: core biomarkers reflect Alzheimer’s-specific pathology, and non-core biomarkers, include non-specific markers involved in Alzheimer’s pathogenesis and markers of common non-Alzheimer’s co-pathologies:
Core Biomarkers
- Core 1 biomarkers are considered sufficient for an Alzheimer’s diagnosis when combined with clinical history and cognitive testing. These include:
- Amyloid PET scans
- CSF measures such as Aβ42/40, p-tau181/Aβ42, and t-tau/Aβ42
- Select blood tests with at least 90% overall accuracy in detecting abnormal amyloid PET, or those with diagnostic performance equivalent to approved CSF assays
- Core 2 biomarkers are not diagnostic on their own but, when combined with Core 1 biomarkers, they help stage disease severity, assess the likelihood that symptoms are due to Alzheimer’s disease, and estimate progression risk. These include:
- Tau PET scans
- CSF markers, such as MTBR-tau243 and other forms of phosphorylated tau
Non-Core Biomarkers
- Non-core biomarkers account for the biological heterogeneity of Alzheimer’s disease and the presence of common co-pathologies in the aging population. These biomarkers reflect disease processes beyond amyloid and tau pathology:
- I (Inflammation): CSF or plasma GFAP
- V (Vascular injury): white matter hyperintensities observed on MRI
- S (α-synuclein pathology): CSF α -synuclein seed amplification assay
- N (Neurodegeneration markers): FDG-PET and MRI-based brain atrophy, as well as CSF or plasma NfL
How are these biomarkers measured?
There are three main methods for measuring Alzheimer’s biomarkers: PET scans, cerebrospinal fluid tests, and blood tests. Each approach comes with trade-offs in terms of accuracy, cost, and accessibility.
- PET scans use radioactive tracers to visualize the levels of beta-amyloid, tau, or glucose metabolism in the brain. Currently, multiple amyloid tracers have been authorized by the FDA and Medicare typically covers one amyloid PET scan during the initial diagnostic work-up.3 Tau and FDG scans may cost $1,800 to $3,000 and are often paid out of pocket. Only one tracer is measured at a time and guidelines specify a minimum period between PET scans.4,5
- CSF tests involve a lumbar puncture to extract a patient’s CSF. An immunoassay test is used to measure amyloid and tau protein fragments that reflect brain pathology.6 Unlike PET scans, FDA-authorized CSF immunoassays tests can simultaneously measure both amyloid and tau biomarkers from the same sample. Several of these tests are covered by Medicare, in many cases, however reimbursement does not adequately cover the cost of the procedure for the physician.7
- Blood tests are the newest, least invasive, and most scalable method to detect Alzheimer’s disease biomarkers. These tests measure the levels of various proteins in blood plasma using different technologies, such as immunoassays and mass spectrometry. Similar to CSF tests, blood tests can measure multiple biomarkers at once. Some of these tests have demonstrated up to 90% sensitivity and specificity and comparable performance to CSF tests.8,9 Medicare reimbursement is not yet available.10 While patients often prefer PET scans due to their non-invasive nature, CSF and blood tests offer critical insights — particularly as more affordable and accessible blood-based diagnostics become increasingly available.
Can biomarkers alone confirm Alzheimer’s?
Experts, including members of the International Working Group, caution against relying solely on biomarkers.11 They argue that Alzheimer’s should be defined as a clinical-biological construct — meaning both symptoms and biological evidence are important.
Currently, neurologists do not recommend testing asymptomatic patients who do not have a hereditary form of Alzheimer’s disease. Biomarkers alone cannot reliably predict which healthy individuals will develop Alzheimer’s disease, and no preventive therapies have yet been developed.
The takeaway for clinical practice
The A/T/N framework and the Revised Criteria for Diagnosis and Staging of Alzheimer’s disease provide clinicians with a biology-based approach to support diagnostic evaluation and disease staging. PET scans, CSF assays, and emerging blood tests can now detect biomarker changes that reflect key hallmarks of the disease, including amyloid plaque deposition, tau pathology and associated neurodegeneration — allowing for earlier detection and more precise assessment for Alzheimer’s pathology.
Today, these biomarkers are helping clinicians diagnose Alzheimer’s disease sooner and provide patients and doctors with a more accurate prognosis. Core 1 biomarkers confirm the biological presence of Alzheimer’s pathology, Core 2 biomarkers provide complementary information about disease progression, and non-core biomarkers offer additional context on brain health and co-existing conditions.
Both the International Working Group and Alzheimer’s Association Working Group emphasize that biomarker testing is not currently recommended for use in asymptomatic individuals. However, when used in symptomatic patients, these biomarkers add precision and provide a fuller picture of brain health. Together, they’re reshaping how clinicians detect, and treat the disease.
References:
- Jack CR, Bennett DA, Blennow K, et al. A/T/N: An unbiased descriptive classification scheme for Alzheimer disease biomarkers. Neurology. 2016;87(5):539-547. doi:10.1212/WNL.0000000000002923
- Jack CR, Andrews JS, Beach TG, et al. Revised criteria for diagnosis and staging of Alzheimer’s disease: Alzheimer’s Association Workgroup. Alzheimer’s & Dementia. 2024;20(8):5143-5169. doi:10.1002/alz.13859
- Rabinovici GD, Knopman DS, Arbizu J, et al. Updated appropriate use criteria for amyloid and tau pet: a report from the Alzheimer’s association and society for nuclear medicine and molecular imaging workgroup. Journal of Nuclear Medicine. Published online January 8, 2025. doi:10.2967/jnumed.124.268756
- Evaluating the cost and benefit of amyloid PET scans and new Alzheimer disease therapies: A financial and clinical perspective. MedLink Neurology; 2024. URL: www.medlink.com/news/evaluating-the-cost-and-benefit-of-amyloid-pet-sca…
- Berger M, Gould MK, Barnett PG. The cost of positron emission tomography in six united states veterans affairs hospitals and two academic medical centers. American Journal of Roentgenology. 2013;181(2):359-365. doi:10.2214/ajr.181.2.1810359
- Shaw LM, Arias J, Blennow K, et al. Appropriate use criteria for lumbar puncture and cerebrospinal fluid testing in the diagnosis of Alzheimer’s disease. Alzheimer’s & Dementia. 2018;14(11):1505-1521. doi:10.1016/j.jalz.2018.07.220
- Hampel H, Shaw LM, Aisen P, et al. State‐of‐the‐art of lumbar puncture and its place in the journey of patients with Alzheimer’s disease. Alzheimer’s Dementia. 2022;18(1):159-177. doi:10.1002/alz.12372
- Palmqvist S, Tideman P, Mattsson-Carlgren N, et al. Blood biomarkers to detect Alzheimer disease in primary care and secondary care. JAMA. 2024;332(15):1245. doi:10.1001/jama.2024.13855
- Arranz J, Zhu N, Rubio-Guerra S, et al. Diagnostic performance of plasma pTau217, pTau181, Aβ1-42 and Aβ1-40 in the LUMIPULSE automated platform for the detection of Alzheimer disease. Alzheimer’s Research & Therapy. 2024;16(1):139. doi:10.1186/s13195-024-01513-9
- Peterson E. Who’s paying for those blood-based biomarker tests for Alzheimer’s disease? Neurology Today. 2024;24(22):1,23-24. doi:10.1097/01.wnt.0001095436.22662.2c
- Dubois B, Villain N, Schneider L, et al. Alzheimer disease as a clinical-biological construct—an international working group recommendation. JAMA Neurol. 2024;81(12):1304. doi:10.1001/jamaneurol.2024.3770