On November 3, 1906, the German clinical psychiatrist and neuroanatomist Alois Alzheimer reported “A...
Understanding the Aβ1-42/Aβ1-40 ratio in relation to Alzheimer’s Disease
Jul 29, 2020
Dr. Rianne Esquivel and Dr. Francesca De Simone | Fujirebio Diagnostics Inc adapted from Dr. Sandra Langer et al., Fujirebio Europe February 2019
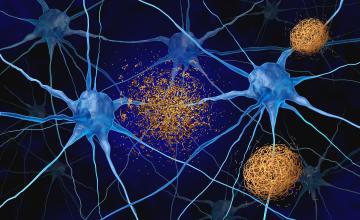
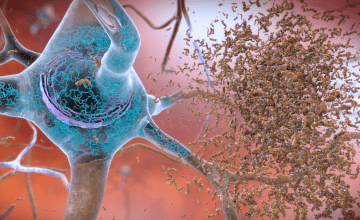
It is widely agree that, since cerebrospinal fluid (CSF) is in direct contact with the central nervous system (CNS), analytes measured in CSF can be considered potential biomarkers for neurodegenerative diseases if thoroughly validated and accepted parameters are used. CSF biomarkers that come closest to fulfilling these criteria are amyloid β peptides (Aβ peptides) and Tau proteins. This can easily be explained by the involvement of these proteins in pathologic events associated with neurodegenerative disease, namely deposition of senile plaques and formation of neurofibrillary tangles. Involvement of these proteins in Alzheimer’s disease (AD) is known and has been investigated intensively for many years. However, there is no single marker that can differentiate AD from other neurodegenerative disorders or predict the risk of progression to AD. This guidance paper will summarize some potential uses of CSF amyloid β peptides ending at positions 42 and 40 (Aβ1-42 and Aβ1-40, respectively) in combination as an Aβ1-42/Aβ1-40 ratio and demonstrate that:
- it is significantly better than CSF Aβ1-42 alone at detecting brain amyloid deposition
- it may help to differentiate amyloid deposition due to AD dementia from non-AD dementias
- it reduces variability due to preanalytical differences.
CSF Aβ1-42/Aβ1-40 ratio as a potential tool to detect amyloid deposition
A study by Wiltfgang et al. found that in a population of cognitively normal individuals and individuals with AD, the distribution of total Aβ (40 and 42) follows a Gaussian distribution, with Aβ1-40 making up about 70% of total Aβ load.1 Although most cases fell within +/- 2SD of the Gaussian distribution, with the majority having normal total Aβ, outliers were still present. Some individuals had high total Aβ and some had low total Aβ. This was true for both normal and AD subjects.
This means that AD patients with a high total Aβ load could be identified incorrectly as amyloid negative and vice versa; normal subjects with low total Aβ could be diagnosed as amyloid positive, if only Aβ1-42 is used.
In all three manifestations of amyloid production (normal, low, and high total Aβ) the ratio could correctly interpret abnormal amyloid deposition in more cases than Aβ1-42 alone.
In a proof-of-principle study carried out in 2007, Wiltfang et al. concluded that the amyloid β concentration ratio should replace the ‘raw’ concentrations of corresponding Aβ peptides to improve reliability of the neurochemical dementia diagnosis2.
More recently, several studies demonstrated added value for CSF Aβ1-40 or the CSF Aβ1-42/Aβ1-40 ratio to distinguish AD when presented with ambiguous AD CSF biomarker profiles3–5. Dementia with Lewy bodies (DLB), the second most common dementia in the elderly, after Alzheimer’s disease (AD), presents similar symptoms to AD, making clinical differentiation difficult. A retrospective analysis from Bousige et al. found that Aβ1-42/1-40 concentrations observed in DLB were clearly distinct from AD Aβ1-42/1-40 concentrations at both early and late stages of disease, whereas concentrations of Aβ1-42 alone in patients with demented DLB overlapped with those seen in AD.
These and other results show that use of the Aβ1-42/1-40 ratio significantly improves understanding of amyloid deposition over the use of Aβ1-42 alone.
FDI-589 06/20