On November 3, 1906, the German clinical psychiatrist and neuroanatomist Alois Alzheimer reported “A...
Everything You Need to Know About Amyloid Presence and Alzheimer’s Disease-modifying Therapies
Jun 25, 2025
Confirming amyloid pathology before administering Alzheimer’s disease-modifying therapies.
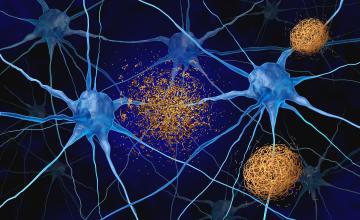
Approximately seven million Americans are currently living with Alzheimer’s disease (AD).¹ Clinicians must confirm amyloid pathology and rule out other potential causes of cognitive impairment before determining the best course of treatment. Once Alzheimer’s disease is established, clinicians have a new generation of treatments to consider: An estimated 2.2 million of those diagnosed with AD may be eligible for one of two newly approved disease-modifying therapies (DMTs). This new class of anti-amyloid drugs is designed to reduce AD-related amyloid pathology in the disease’s earliest symptomatic stages.2
Some patients may be at a higher risk of adverse side effects depending on factors such as genetic status.2,3 Here’s what you need to know about confirming Alzheimer's disease pathology and prescribing these new DMTs.
3 ways to confirm Alzheimer’s amyloid pathology
After a clinical evaluation that rules out other causes of cognitive decline — e.g., vitamin B12 deficiency, thyroid dysfunction, medications, long COVID, depression, or other neurodegenerative diseases4 — one or more of the following tests is typically used to confirm AD pathology:
PET imaging
- PET brain imaging utilizes a radioactive tracer that binds to beta-amyloid (β-Amyloid) plaques or tau neurofibrillary tangles in the brain.
- There are three FDA-approved fluorine-18 radiotracers available: 18F-florbetapir, 18F-flutemetamol, 18F-florbetaben. Each is visually interpreted, with slight differences in color scale and positivity criteria depending on the agent used.5
- A tau PET tracer, 18F-flortaucipir, was approved by the FDA in 2020. 6 While not used to confirm Alzheimer’s pathology for diagnostic purposes, tau PET may support disease staging and prognosis, as outlined in the 2024 revised diagnostic criteria.7 Additionally, its use to determine treatment eligibility is not addressed in the FDA prescribing information for current DMTs. 5
- Medicare covers amyloid and tau PET scans. 5
Cerebrospinal fluid testing
- Measures key biomarker ratios in CSF, including: pTau 181/β-Amyloid 1-42, β-Amyloid 1-42/40, and tTau/Aβ428
- May be covered by Medicare in certain clinical contexts 9
Blood-based biomarker testing
- Several blood tests are available in the U.S. as laboratory-developed tests (LDTs).
- On May 16, 2025, the FDA cleared the first plasma-based in vitro diagnostic (IVD) test, the Lumipulse® G pTau 217/ β-Amyloid 1-42 Plasma Ratio.11
- Test results are reported as a quantitative value, which is compared to pre-defined cutoffs to determine a positive, negative, or indeterminate result.
- Medicare reimbursement via specific billing codes for many of these tests is being developed and should be available by January 2026.
Some blood-based Alzheimer’s biomarker tests are intended for triage use: meaning they are designed to only rule out Alzheimer’s disease. A negative result suggests the individual is unlikely to have amyloid pathology. However, a positive or inconclusive result requires follow-up testing with either CSF analysis or amyloid PET imaging.
In this case, the Blood Biomarker Workgroup for the Global CEO Initiative on Alzheimer’s Disease recommends using a test with a sensitivity of≥90%, and a specificity of≥85% in primary care settings or 75–85% in specialist settings.10
Other blood-based tests are intended as confirmatory use, offering sufficient precision and accuracy to confirm amyloid pathology without additional testing. For this purpose, guidelines recommend that these tests have a sensitivity and specificity of approximately ≥ 90%.10
Fujirebio’s blood-based biomarker test
In May, the FDA approved Fujirebio’s Lumipulse® G pTau 217/β-Amyloid 1-42 Plasma Ratio blood test for use in adults aged 50 and older presenting in a specialist setting with cognitive complaints.11
The test measures the levels of pTau-217, a phosphorylated form of the tau protein that increases in the presence of amyloid pathology associated with Alzheimer’s disease, and β-Amyloid 1-42, which is a proteolytic fragment of the amyloid precursor protein (APP) and a major component of amyloid plaques. A decrease in soluble Aβ42 levels reflects its aggregation in plaques, indicating underlying amyloid pathology. An elevated pTau 217/ β-Amyloid 1-42 plasma ratio is associated with the presence of amyloid plaques in the brain, and correlates strongly with amyloid pathology in the brain.
In conjunction with other patient clinical information, the test has proven accurate enough to confirm amyloid pathology.11
Leqembi vs. Kisunla
- There are currently two FDA-approved DMTs, Eisai and Biogen’s Leqembi (lecanemab) and Eli Lilly’s Kisunla (donanemab). They are the only two FDA-approved monoclonal antibodies currently available to target and clear beta amyloid plaques in order to help slow the progression of Alzheimer’s cognitive and functional decline.12,13
- Currently, both DMTs require intravenous infusion, although subcutaneous delivery systems are under review by the FDA for Leqembi.12,13,14
Mechanism of action
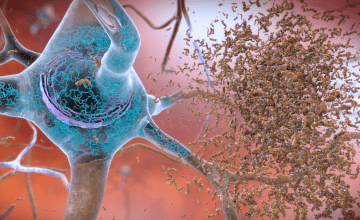
- Leqembi primarily targets soluble beta-amyloid protofibrils and also binds to insoluble fibrils associated with plaques.15 Its epitope was first characterized in a Northern Swedish family with the Arctic mutation, a genetic variant linked to early-onset Alzheimer’s.16
- Kisunla binds to N-terminal pyroglutamate-modified β-Amyloid fibrils (pGlu3-Aβ), which are prone to aggregation.17,18
Although they bind to different conformations of β-Amyloid, both therapies promote microglia-mediated plaque clearance. 17 The resulting reduction in amyloid burden can be monitored via amyloid PET imaging.
Effectiveness and limitations
In Phase 3 trials, both drugs showed modest benefits in slowing cognitive decline, with stronger effects observed in patients treated during the mild cognitive impairment (MCI) stage:
- Leqembi showed a 0.45-point reduction in the decline of the Clinical Dementia Rating – Sum of Boxes (CDR-SB) compared to placebo over 18 months12
- Kisunla showed a 0.7-point reduction in CDR-SB over 76 weeks compared to placebo13
However, these effects fall below the minimal clinically important difference (MCID) established in prior studies.19,20 Further, subgroup analyses suggest Leqembi had reduced efficacy in women and ApoE4 homozygotes.21,22
Regulatory notes: Leqembi received conditional approval in Europe for non-homozygote patients only. The European Medicines Agency has not recommended approval of Kisunla. 23,24
Adverse events: Risk of ARIA
Both therapies are associated with amyloid-related imaging abnormalities (ARIA), which may include edema (ARIA-E) or microhemorrhage (ARIA-H). Most ARIA events are asymptomatic. About 0.7–6% of ARIA cases present with symptoms.12,13
- Leqembi: ARIA-E occurred in 12.6% of patients, and ARIA-H in 17.3%.12
- Kisunla: ARIA-E occurred in 24% of patients, and ARIA-H in 31%.13
- ApoE4 homozygotes had a higher incidence of ARIA, with risk approximately twofold greater than in non-carriers.12,13
Anticoagulant use can also increase a person’s risk of ARIA.25 These therapies carry an increased risk in patients with certain MRI findings. In particular, pretreatment microhemorrhages and superficial siderosis have been associated with an increased risk of ARIA in clinical trials of Leqembi and Kisunla.25,26,27
Severe complications were rare in both trials but included cases of intracerebral hemorrhage and fatal outcomes.
For a comprehensive list of ARIA risk factors and eligibility restrictions, refer to the FDA-approved prescribing information for each drug.28,29
Administration and monitoring
- Leqembi: administered at 10mg/kg via intravenous infusion every two weeks, over approximately 30–60 minutes.28 While the pivotal trial followed patients for 18 months, the FDA label does not specify a treatment duration.12,28 A subcutaneous maintenance formulation is currently under FDA review.14
- Kisunla: initiated with 700mg IV every four weeks for the first three doses, followed by 1400mg every four weeks.29 Each dose is infused over approximately 30 minutes.29 Treatment is discontinued once the amyloid plaque burden falls below a prespecified threshold, as determined by amyloid PET imaging.29 Lilly is also studying reduced Kisunla dosing to lower ARIA risk while maintaining efficacy.30
MRI monitoring guidelines:
- Leqembi: MRI scans are recommended after the 5th, 7th, and 14th infusion; For ApoE4 carriers, an additional MRI is advised prior to the 26th infusion.26,28
- Kisunla: MRI scans should be performed before the 2nd, 3rd, 4th, and 7th infusions. High-risk patients require additional scans before infusion number 12th.27,29
Cost and coverage
- Leqembi: List price is $26,500 per year for a patient weighing approximately 165 pounds (75kg), based on a biweekly 10mg/kg IV infusion regimen.31
- Kisunla: List price is approximately $32,000 per year; total cost depends on treatment duration.32
Currently, Medicare covers both therapies, although coverage criteria apply. Private insurer coverage varies and may depend on documentation of diagnostic confirmation.33
A recap: Prescribing DMTs for Alzheimer’s
Recent advances in biomarker testing will streamline the evaluation process for DMTs, enabling clinicians to confirm amyloid pathology more efficiently and identify appropriate candidates.34 Currently, amyloid PET imaging and CSF testing remain the primary tools used to confirm amyloid pathology and meet the diagnostic eligibility criteria for Leqembi or Kisunla. However, with the emergence of validated blood-based biomarkers, plasma testing is expected to become a standard component of the clinical workup in the near future.
References:
-
2024 Alzheimer’s Disease Facts and Figures. Alzheimer’s Association. (2024) URL: https://www.alz.org/getmedia/76e51bb6-c003-4d84-8019-e0779d8c4e8d/alzhe… s-and-figures.pdf
- Dittrich, Anna, et al. Proportion of community-dwelling individuals older than 70 years eligible for lecanemab initiation: the Gothenburg H70 Birth Cohort Study. Neurology102.9 (2024): e209402. doi:10.1212/WNL.0000000000209402
- Foley, K. E., & Wilcock, D. M. (2024). Three major effects of APOEε4 on Aβ immunotherapy induced ARIA. Frontiers in Aging Neuroscience, 16, 1412006. doi: 10.3389/fnagi.2024.1412006
- Anand S, Schoo C. Mild Cognitive Impairment. [Updated 2024 Jan 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK599514/
- Rabinovici GD, Knopman DS, Arbizu J, Benzinger TLS, Donohoe KJ, Hansson O, Herscovitch P, Kuo PH, Lingler JH, Minoshima S, Murray ME, Price JC, Salloway SP, Weber CJ, Carrillo MC, Johnson KA. Updated appropriate use criteria for amyloid and tau PET: A report from the Alzheimer's Association and Society for Nuclear Medicine and Molecular Imaging Workgroup. Alzheimer’s & Dementia. 2025 Jan;21(1):e14338. doi: 10.1002/alz.14338
- Vermeiren, Marie R., et al. "Survey among experts on the future role of tau‐PET in clinical practice and trials." Alzheimer's & Dementia: Diagnosis, Assessment & Disease Monitoring 16.4 (2024): e70033. doi:10.1002/dad2.70033
- Jack CR, Andrews JS, Beach TG, et al. Revised criteria for diagnosis and staging of Alzheimer's disease: Alzheimer's Association Workgroup. Alzheimer's Dement. 2024; 20: 5143–5169. doi: 10.1002/alz.13859
- Barthélemy, N.R., Salvadó, G., Schindler, S.E. et al. Highly accurate blood test for Alzheimer’s disease is similar or superior to clinical cerebrospinal fluid tests. Nat Med 30, 1085–1095 (2024). https://doi.org/10.1038/s41591-024-02869-z
- Deverka PA, Lin GA, Phillips KA. Payer Coverage Considerations for Alzheimer Disease Blood-Based Biomarker Tests. JAMA. 2024;332(22):1877-1878. doi:10.1001/jama.2024.19084
- Schindler SE, Galasko D, Pereira AC, Rabinovici GD, Salloway S, Suárez-Calvet M, Khachaturian AS, Mielke MM, Udeh-Momoh C, Weiss J, Batrla R, Bozeat S, Dwyer JR, Holzapfel D, Jones DR, Murray JF, Partrick KA, Scholler E, Vradenburg G, Young D, Algeciras-Schimnich A, Aubrecht J, Braunstein JB, Hendrix J, Hu YH, Mattke S, Monane M, Reilly D, Somers E, Teunissen CE, Shobin E, Vanderstichele H, Weiner MW, Wilson D, Hansson O. Acceptable performance of blood biomarker tests of amyloid pathology - recommendations from the Global CEO Initiative on Alzheimer's Disease. Nature Reviews Neurol. 2024 Jul;20(7):426-439. doi: 10.1038/s41582-024-00977-5.
- FDA Clears First Blood Test Used in Diagnosing Alzheimer’s Disease. FDA. (2025): URL: https://www.fda.gov/news-events/press-announcements/fda-clears-first-blood-testhttps://www.fda.gov/news-events/press-announcements/fda-clears-first-blood-test-used-diagnosing-alzheimers-diseaseuseddiagnosing-alzheimers-disease
- Van Dyck, Christopher H., et al. Lecanemab in early Alzheimer’s disease. New England Journal of Medicine 388.1 (2023): 9-21. doi:10.1056/NEJMoa2212948
- Sims, John R., et al. Donanemab in early symptomatic Alzheimer disease: the TRAILBLAZER-ALZ 2 randomized clinical trial. JAMA 330.6 (2023): 512-527. doi:10.1001/jama.2023.13239
- FDA Accepts LEQEMBI® (lecanemab-irmb) Biologics License Application for Subcutaneous Maintenance Dosing for the Treatment of Early Alzheimer’s Disease. Eisai. (2024) URL: https://www.eisai.com/news/2025/news202502.html
- Johannesson M, Söderberg L, Zachrisson O, et al. Lecanemab demonstrates highly selective binding to Aβ protofibrils isolated from Alzheimer's disease brains. Mol Cell Neurosci. 2024;130:103949. doi:10.1016/j.mcn.2024.103949
- Nilsberth, C., Westlind-Danielsson, A., Eckman, C. et al. The 'Arctic' APP mutation (E693G) causes Alzheimer's disease by enhanced Aβ protofibril formation. Nature Neurosci 4, 887–893 (2001). doi:10.1038/nn0901-887
- Loeffler DA. Antibody-Mediated Clearance of Brain Amyloid-β: Mechanisms of Action, Effects of Natural and Monoclonal Anti-Aβ Antibodies, and Downstream Effects. J Alzheimers Dis Rep. 2023 Aug 14;7(1):873-899. doi:10.3233/ADR-230025.
- He, Weilan, Barrow, CJ. The Aβ 3-pyroglutamyl and 11-pyroglutamyl peptides found in senile plaque have greater β-sheet forming and aggregation propensities in vitro than full-length Aβ. Biochemistry 38.33 (1999): 10871-10877. doi:10.1021/bi990563r
- Muir, Ryan T., et al. Minimal clinically important difference in Alzheimer's disease: Rapid review. Alzheimer's & Dementia 20.5 (2024): 3352-3363. doi:10.1002/alz.13770
- Andrews JS, Desai U, Kirson NY, Zichlin ML, Ball DE, Matthews BR. Disease severity and minimal clinically important differences in clinical outcome assessments for Alzheimer's disease clinical trials. Alzheimer's Dement (N Y). 2019 Aug 2;5:354-363. doi:10.1016/j.trci.2019.06.005.
- Daniel Andrews, Simon Ducharme, Howard Chertkow, Maria Pia Sormani, D. Louis Collins. The higher benefit of lecanemab in males compared to females in CLARITY AD is probably due to a real sex effect. Alzheimer's & Dementia, 2025; 21 (1) DOI: 10.1002/alz.14467
- Kurkinen M. Lecanemab (Leqembi) is not the right drug for patients with Alzheimer's disease. Adv Clin Exp Med. 2023;32(9):943-947. doi:10.17219/acem/171379
- Commission authorises medicine for treatment of early Alzheimer’s disease. European Commission Health and Food Safety. (2025). URL: https://ec.europa.eu/newsroom/sante/items/879055/en
- Kisunla. European Medicines Agency. (2025). URL: https://www.ema.europa.eu/en/medicines/human/EPAR/kisunla
- Doran SJ, Sawyer RP. Risk factors in developing amyloid related imaging abnormalities (ARIA) and clinical implications. Front Neurosci. 2024 Jan 19;18:1326784. doi:10.3389/fnins.2024.1326784
- Cummings, J., et al. Lecanemab: appropriate use recommendations. The Journal of Prevention of Alzheimer's Disease 10.3 (2023): 362-377. doi:https://doi.org/10.14283/jpad.2023.30
- Rabinovici, G. D., et al. Donanemab: appropriate use recommendations. The Journal of Prevention of Alzheimer's Disease 12(5) 2025: 100150. doi:10.1016/j.tjpad.2025.100150
- Highlights of Prescribing Information. Drugs@FDA. https://www.accessdata.fda.gov/drugsatfda_docs/label/2023/761269Orig1s001lbl.pdf
- Highlights of Prescribing Information. Eli Lilly. https://uspl.lilly.com/kisunla/kisunla.html#pi
- Modified Titration of Donanemab Demonstrated Reduction of ARIA-E in Early Symptomatic Alzheimer's Disease Patients in Phase 3b study. Eli Lilly. (2024). URL: https://investor.lilly.com/news-releases/news-release-details/modified-titration-donanema b-demonstrated-reduction-aria-e-early
- Eisai’s approach to U.S. Pricing for leqembi™ (lecanemab), a treatment for early alzheimer’s disease, sets forth our concept of “societal value of medicine” in relation to “price of medicine”. Eisai. (2023). URL: https://www.eisai.com/news/2023/news202302.html
- Lilly's Kisunla™ (donanemab-azbt) Approved by the FDA for the Treatment of Early Symptomatic Alzheimer's Disease. Eli Lilly. (2024). URL: https://investor.lilly.com/newshttps://investor.lilly.com/news-releases/news-release-details/lillys-kisunlatm-donanemab-azbt-approved-fda-treatment-earlyreleases/news-release-details/lillys-kisunlatm-donanemabazbt-approved-fda-treatmenthttps://investor.lilly.com/news-releases/news-release-details/lillys-kisunlatm-donanemab-azbt-approved-fda-treatment-earlyearly
- Murphy T. Insurers won’t cover new Alzheimer’s treatment for some customers. AP News. (2023). URL: https://apnews.com/article/leqembi-insurance-coverage-alzheimerhttps://apnews.com/article/leqembi-insurance-coverage-alzheimer-ec7fcdf99ceaaa60ad1cee737c0b7ecbec7fcdf99ceaaa60ad1 cee737c0b7ecb
- Mattke S, et al. Impact of a High-Performing Blood Test on Wait Times for Determination of Eligibility for a Disease-Modifying Alzheimer’s Treatment in the U.S. Presented at: 2024 Alzheimer’s Association International Conference; July 18 to August 1; Philadelphia, Pennsylvania. Abstract 91612.