Better care for pregnant women diagnosed with precancerous cervical lesions
By Rebecca Millecamps, Fujirebio
The article below is part of a series of resources dedicated to the state-of-the-art of HPV testing.
Get a full overview of our resources here.
Cervical cancer is the most common malignancy of the female reproductive tract during pregnancy occurring in 1 to 10 per 10 000 pregnancies with an incidence of 0.02% to 0.9%. In recent years, the incidence of cervical intraepithelial neoplasia (CIN) diagnosed in unvaccinated pregnant women has substantially increased. This is related to a general increase in the prevalence of CIN in women of reproductive age.1 The highest incidence of high-grade intraepithelial lesions (HSILs; CIN2/3) is found among women aged 25-35 and thus in the reproductive age group.2
Literature provides widely varying data regarding regression, persistence, and progression of CIN3 lesions during pregnancy. This may be due to differences in study population regarding size and age as well as diagnostics performed during pregnancy. Despite these varying results, it can be stated that progression of CIN to invasive carcinoma in pregnancy is rare. A wait-and-see approach may therefore be justified. Postpartum follow-up and, if necessary, treatment of the lesions are essential.3
Overexpression of sex hormones during pregnancy may facilitate cervical carcinogenesis by induction of squamous metaplasia in the transformation zone and by modifications in the local immune system. The decrease in sex hormones after delivery might explain increased regression. There have been various attempts to explain the increase in regression after vaginal delivery as observed in several studies.2
Management of CIN diagnosed during pregnancy has changed but is still far from perfect
There is a clear evolution from surgical treatment to a more conservative follow-up approach with repeated Pap smear, colposcopy and in case of cancer suspicion a biopsy at regular intervals to rule out invasive disease.1
This approach is better than the historical management with excisional treatment of any CIN3+ lesion in pregnancy, but still far from perfect.1
Cytology is subjective and the relatively low specificity of cytology and HPV among young women leads to unnecessary over-referral, overtreatment and anxiety in pregnant women.1
Pregnancy-associated changes of the cervix may complicate the interpretation of Pap smears and lead to an overall higher rate of false-positive results. Diagnosis of CIN3 or cervical cancer is made by colposcopy and biopsy. Also colposcopy in pregnant women is more challenging than in non-pregnant women e.g. because of mucus overproduction, contact bleeding, etc. as a result of hormonal changes. Colposcopy, cytology and histology should be performed and evaluated by experienced examiners. Treatment depends on evaluation of all findings together and the patient’s informed consent.2,3
Diagnosis of precancerous cervical lesions during pregnancy is a major challenge
Undeniably, the diagnosis of cervical dysplasia during pregnancy is a major challenge for both the patient and the multidisciplinary team in charge, in order to find an individual treatment that does no harm to neither the woman nor her unborn child. 1,3 Treatment increases the risk of pregnancy termination in the second trimester and preterm labor, and perinatal complications. 5
Improved triage markers to predict the course of the CIN lesion during the pregnancy and postpartum would be helpful to safely manage the pregnant women with a conservative follow-up until after delivery.1
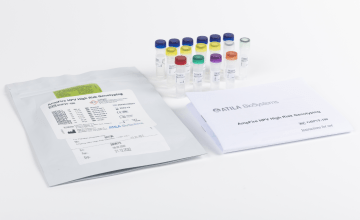
Methylation levels provide information on severity of the precancer
The performance of the FAM19A4/miR124-2 methylation test for triage of CIN3+-diagnosed pregnant women was evaluated in a German multicenter study. Biopsy material was collected from CIN3+-diagnosed pregnant women with known clinical course over time as well in cross-section setting.1
All pregnant women with cervical cancer and with CIN3 progressing to cancer tested positive for FAM19A4/miR124-2 methylation (100%, 22/22). In the regressing CIN3 group 47.5% and in the group without CIN 21.6% tested methylation positive. High volume CIN3 and random selected CIN3 were methylation-positive in 91.7% and 82.1%, respectively. Methylation levels were significantly higher in progressive CIN3 and cancer compared to the controls.1
A negative FAM19A4/miR124-2 methylation test can rule out progressive CIN disease in pregnant women diagnosed with CIN3. This can help the clinician to safely manage pregnant women with conservative follow-up until after delivery.1
Nonpregnant women also benefit from a more conservative approach
Most CIN lesions, particularly in young women (<30 years), regress spontaneously. Active surveillance, rather than immediate medical intervention, is therefore justified, especially among young women who are likely to adhere to monitoring. Conservative management with active surveillance, instead of immediate local excision, is justified in selected women, especially if future pregnancies are considered and compliance with surveillance is likely to be high.4
The age of women having their first child is increasing, and women are more often diagnosed with CIN2/3 before their first pregnancy. It is shown that excisional techniques are associated with an increased risk of pre-term birth and also other short-and long-term complications. Treating only those with disease that has a true progressive potential is of utmost importance.5
The FAM19A4/miR124-2 methylation test in HPV-positive women aged <30 years has recently been evaluated, together with HPV16/18 genotyping, aiming to identify CIN2/3 lesions in need of treatment. The FAM19A4/miR124-2 methylation test result reflects the nature (i.e., high or low short-term cancer progression risk) of the underlying CIN, thereby providing guidance for the treatment policy in women with CIN2/3. In conclusion of this study, compared with HPV16/18 genotyping, the FAM19A4/miR124-2 methylation test detects non-productive, transforming CIN2/3 lesions with high specificity in women aged <30 years, providing clinicians supportive information about the need for treatment of CIN2/3 in young HPV-positive women.6
Accumulated evidence on DNA methylation from key studies
Summarizing the current knowledge regarding conservative CIN2 management shows that DNA methylation is an accurate predictor of disease progression and a valid triage tool for HPV-positive women with CIN2, performing better than cytology.5
Considering the accumulated evidence from key studies, FAM19A4/miR124-2 methylation may be used as a valid triage method for screen-positive women because it provides a very high negative predictive value for the development of cervical cancer. In addition, it may be particularly useful in distinguishing younger women with high-risk lesions that do not need immediate surgical treatment. 5
References:
- Hampl M, Hesselink AT, Meijer CJLM, et al. Evaluation of FAM19A4/miR124-2 methylation performance in the management of CIN3 diagnosed pregnant women. Int J Cancer. 2022; 151(9): 1578-1585. https://doi.org/10.1002/ijc.34153
- Stuebs FA, Mergel F, Koch MC, et al. Cervical intraepithelial neoplasia grade 3: development during pregnancy and postpartum. Arch Gynecol Obstet. 2023; 307, 1567-1572. https://doi.org/10.1007/s00404-022-06815-7
- Freudenreich R, Weiss M, Engler T, et al. Characterization and clinical management of abnormal cytology findings in pregnant women: a retrospective analysis. Arch Gynecol Obstet. 2022; 306, 2017-2026. https://doi.org/10.1007/s00404-022-06699-7
- Tainio K, Athanasiou A, Tikkinen KAO, et al. Clinical course of untreated cervical intraepithelial neoplasia grade 2 under active surveillance: systematic review and meta-analysis. BMJ. 2018; 360:k499. https://doi.org/10.1136/bmj.k499
- Dovnik A, Poljak M. The Role of Methylation of Host and/or Human Papillomavirus (HPV) DNA in Management of Cervical Intraepithelial Neoplasia Grade 2 (CIN2) Lesions. Int J Mol Sci. 2023; 24(7), 6479. https://doi.org/10.3390/ijms24076479
- Vink FJ, Meijer CJLM, Hesselink AT, et al. FAM19A4/miR124-2 Methylation Testing and Human Papillomavirus (HPV) 16/18 Genotyping in HPV-Positive Women Under the Age of 30 Years. Clin Infect Dis. 2023;76(3):e827-e834. https://doi.org/10.1093/cid/ciac433